Far more than just personal data, PHI is a prime target for cybercriminals, often fetching higher prices on the dark web than even financial details.
With healthcare operations increasingly digitized, PHI navigates a complex, integrated ecosystem. This intricate web, while enabling better care, also creates numerous points of vulnerability.
This is where Data Loss Prevention (DLP) becomes not just important, but essential.
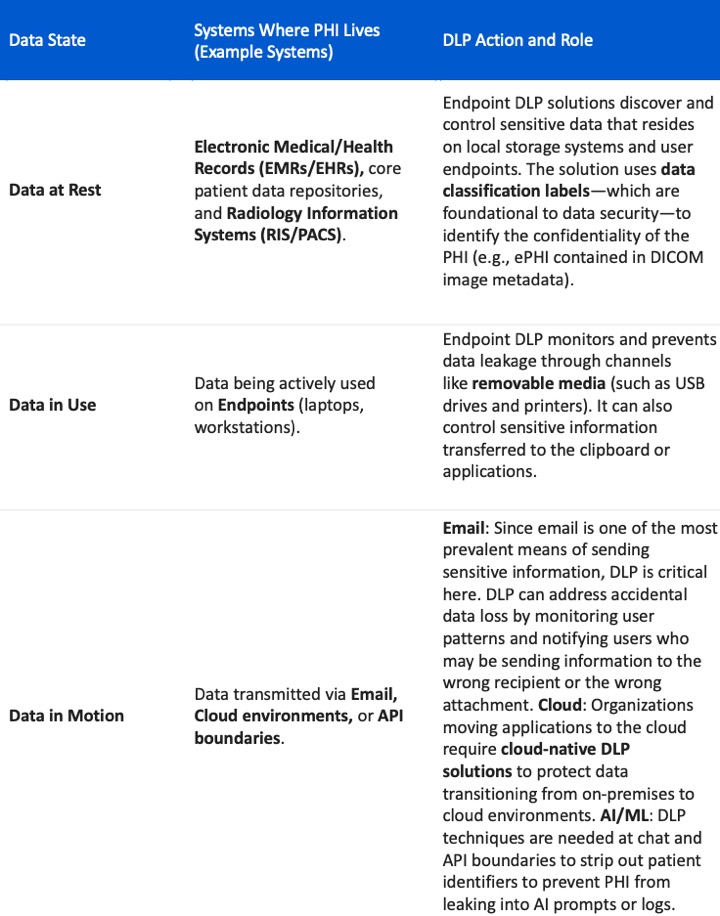
DLP provides crucial visibility into data usage and movement, dynamically enforcing security policies across this entire ecosystem.
It offers critical monitoring, alerting, warning, blocking, and quarantining features designed to prevent the accidental or malicious loss and exposure of sensitive data. Let’s explore where DLP fundamentally intervenes, based on the state of the data.
Addressing Key Vulnerabilities
DLP plays a vital role in mitigating healthcare’s primary risks:
1. Human Error and Negligence: Human error contributes to 74% of all healthcare data breaches. Traditional DLP focuses heavily on content, but modern solutions are converging with Insider Risk Management (IRM). This allows the DLP system to enrich events with a user-centric view, making it simpler to distinguish between malicious and negligent acts of an end user.
2. Exfiltration and Ransomware: Ransomware is the top threat, and 74% of successful victims report data exfiltration. DLP enforces policies based on both the content (PHI/ePHI) and context of the data. If a user attempts an inappropriate action with sensitive PHI, the DLP policy triggers remediation features such as blocking or quarantining the action to prevent the exposure of that sensitive data.
By implementing a comprehensive DLP strategy, we can move beyond reactive controls and establish dynamic enforcement to protect the continuity of care and the sensitive data of our patients.